Today’s blog topic is Hereditary Hemorrhagic Telangiectasia (HHT) in honor of Global HHT Awareness Day. As some of you may know from our more recent blogs, it is important to shine a spotlight on rare diseases. Rare diseases may only affect a small population in comparison to other more common diseases. But when combining all the people suffering from a rare disease, they make up a huge community. At Personalized Cause®, we believe there is power in awareness, and that there is strength in numbers. Like Helen Keller said, “Alone we can do so little, together we can do so much.”
Red and Blue Ribbons for HHT
Personalized Cause® is proud to announce that we now carry a red and blue awareness ribbon for HHT. The pin is available for purchase here. We have a red and blue awareness ribbon that can be personalized with a name, date or message, too (click here).
What is HHT? Global HHT Awareness Day Raises Awareness
Hereditary Hemorrhagic Telangiectasia is also referred to as Osler-Weber-Rendu Syndrome (OWR). HHT is a genetic blood vessel disease that causes bleeding in various parts of the body. HHT, like other diseases, can go misdiagnosed or undiagnosed for years or decades.
The average length of time for someone with HHT to be properly diagnosed is 27 years. This is because many of the symptoms of HHT can masquerade as other health problems. HHT is a genetic condition. It is not uncommon for more than one member of the same family to suffer from HHT. HHT can affect many organs, including the skin, nose, spine, lungs, gastrointestinal tract, liver, and brain. For this reason, it is important to learn about HHT during Global HHT Awareness Day.
What are the symptoms of HHT?
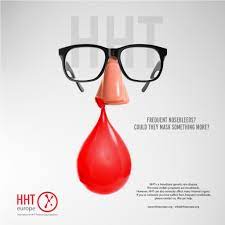
One of the most common symptoms of HHT is frequent nosebleeds. As many as 90 percent of people with HHT experience recurring nosebleeds. Nosebleeds from HHT are caused by malformed blood vessels in the nose. These malformations are called telangiectasia. Telangiectasia itself can be associated with many different health issues. It is actually a common skin condition with causes ranging from sun exposure to disease.
Telangiectasia with HHT tends to affect the lining of the nose, skin, and intestines. They look like little red dots that appear on the surface of the tissue or skin. They are usually 1 to 2 millimeters in diameter, but they are not always visible without magnification. These telangiectasia burst and that is what causes the nose to bleed. Since nosebleeds are not uncommon in healthy people, this symptom is often overlooked by doctors.
Nosebleeds
Nosebleeds caused by HHT typically start around the age of 12, but can start at any time. Onset of HHT nosebleeds range from babies to seniors. The bleeding severity and frequency also vary from patient to patient. For some they may be an annoying inconvenience. Others may experience so much blood loss that they need blood transfusions.
AV Malformations
Another major issue caused by HHT is AVM. AVM stands for arteriovenous malformations. This means that there is a structural abnormality in the connection between an artery and a vein. Arteriovenous malformations are most common in the brain, but they can happen anywhere. HHT causes AVM’s in many different parts of the body, including the brain, lungs, liver, and spine. Each location has different symptoms.
Cerebral AVM’s are not the most common type of AVM due to HHT, but they can be the most dangerous. Approximately 23 percent of people with hereditary hemorrhagic telangiectasia develop a cerebral AVM. Cerebral AVM’s look like a tangle of blood vessels between a vein and an artery. The tangle causes a connection between the vein and artery to grow. This can be dangerous for many reasons. Veins take blood that has already circulated through the brain back to the heart. Arteries take blood full of oxygen from the heart to the brain. Arteries and veins are opposite sides of a two way street. When an AVM is present, it can interfere with this process because the vein and artery connect. This can cause circulation issues, brain damage, neurological symptoms, or even a stroke.
Cerebral Issues
Cerebral AVM’s cause extra pressure in the brain. Over time, this pressure can lead to a thinning or weakening of the blood vessels in the area. If the vessels become weak enough they can burst causing a brain hemorrhage. Bleeding in the brain will cause pressure to increase which causing brain damage. It also prevents parts of the brain from getting oxygen which can be devastating.
Brain AVM’s can cause various symptoms but sometimes cause no symptoms at all. The most common symptoms of AVM are headaches, seizures, or muscle weakness in only one part of the body. If the AVM is large or located in certain areas it can cause more serious symptoms. These symptoms include the symptoms mentioned above but they would be severe. They may also include difficulty balancing, loss of vision, difficulty understanding or speaking. In some cases, they can even cause paralysis.
Pulmonary AVM’s
Pulmonary AVM’s are AVM’s in the lungs. These AVM’s are about twice as common as Brain AVM’s in people with HHT. Around 40-50 percent of patients have them. PAVM’s affect the pulmonary vein and the pulmonary artery. Like brain AVM’s, PAVM’s cause issues with circulation. Because of the location PAVM’s can interfere with the oxygenation of the blood. If there is not enough oxygen in the blood it can cause shortness of breath or difficulty breathing. The lack of oxygen can cause excessive strain during exercise, and may even cause the skin to appear blue.
While it is possible to have a PAVM without having HHT, the vast majority of PAVM’s are caused by HHT. HHT type 1 causes an elevated risk for PAVM’s. PAVM’s can cause brain emboli. A brain embolism is when something in the body becomes dislodged and travels to the brain. It can be a blood clot, clump of bacteria, plaque, or even air bubbles. When they reach the brain they travel through small vessels until they become stuck. This is known as an embolic stroke. Strokes can cause serious disability or death.
Education is Important
Education is key. Global HHT Awareness Day is a time to educate those with HHT and others about living with HHT. People with HHT have to be extra careful when it comes to things that can cause complications from PAVM’s. As I mentioned above, air bubbles and bacteria clumps can cause an embolic stroke. For this reason, people with PAVM’s have to take preventative measures to reduce risk. Air bubbles can occur during surgical procedures, lung trauma, or even scuba diving.
Medical staff are extra careful to make sure people with HHT do not get an air embolism. Scuba diving is not a good idea with a PAVM. Unfortunately, there isn’t any work around. Last, antibiotics are given as a precaution before any medical procedure. Anything that could introduce bacteria into the bloodstream is dangerous without antibiotics. That even includes dental work.
Liver AVM’s
Liver AVM’s (also called liver vascular malformations) can be very common with HHT. Up to 75 percent of people with HHT have a liver AVM, but only around ten percent of those people experience symptoms. Liver AVM’s can cause many symptoms and complications. The majority of symptoms are similar to the symptoms associated with cirrhosis. Severe cases can lead to heart failure due to the continued increased pressure on the heart.
Heart AVM’s
When the heart is affected, diuretics are used to decrease blood volume and swelling. Low sodium diets are a necessity to prevent any extra fluid retention. Sometimes, pressure on the heart can cause heart arrhythmia. There are lots of medicines used to treat this. The last resort for severe cases of liver vascular malformation is a transplant. Liver transplants are only used as a last resort because of the high risk associated. Around ten percent of liver transplant patients do not survive the surgery. The other 90 percent usually see dramatic improvement.
Spinal AVM’s
Last but not least, we have spinal AVM’s. Spinal AVM’s are very rare. They only affect about one percent of people with HHT. Spinal AVM’s can cause tissue damage or death over time because of lack of oxygen to surrounding tissue. This can damage the spine and result in chronic symptoms or disability. A damaged spine can affect your ability to walk or move. It can also cause severe pain, numbness and tingling in your legs. On top of tissue damage, a spinal AVM can swell over time and rupture. This is called a spinal cord hemorrhage. There are surgical treatment options to prevent damage or undo damage. Surgery is not an option for all spinal AVM’s. Most people with a spinal AVM begin to show symptoms by the time they hit their 20’s. The majority of cases are diagnosed in kids under 16 years old.
How is HHT Diagnosed?
HHT is diagnosed using a set of four criteria. If three of the four criteria are met then it is considered a “definite HHT” diagnosis. If there are only two then it is considered a “possible HHT” diagnosis. The criteria for diagnosis are: recurring nose bleeds; telangiectasia in typical HHT areas; diagnosed AVM’s; and a blood relative with “definite HHT”. More symptoms on the criteria list may surface as one gets older. A “possible HHT” diagnosis can become a “definite HHT” diagnosis over time. There is no cure for HHT. Because there is not yet a treatment to treat HHT itself, doctors rely on treating the symptoms. Some treatments may be done to prevent certain complications from arising.
Living with HHT
Living with HHT can be challenging enough on its own. It is made even more difficult by the fact that most people have no idea what it is. Even most physicians don’t know enough about it to correctly diagnose it in its early stages. This is where you come in. Anyone can become an advocate for any cause. All it takes is the desire to make an impact and help others. Something as simple as a Global HHT Awareness Day ribbon can go a long way in spreading awareness.
Awareness Resources for Global HHT Awareness Day
As you may know from looking at our site, we have extensive resources for rare diseases and genetic diseases. In fact, we have compiled specialty lists specifically for each. You can reach them by going to the “find your ribbon” tab in our directory menu. We are currently working on a master list of all causes. The master list will be comprehensive and include brief descriptions, categories and the awareness ribbon color associated with it. It has been a true labor of love. Personalized Cause® prides itself on being the most accurate and up to date awareness resource. Since awareness ribbon colors can change over time, we are researching each cause one by one before we add it to our new master list. Our priority is to ensure that you can trust the information you find on our site. Stay tuned for the Master List arrival later this year.
Sources: CureHHT / MayoClinic / CDC / NORD
